
- #Timely filing limit for all insurance 2021 pdf how to
- #Timely filing limit for all insurance 2021 pdf portable
- #Timely filing limit for all insurance 2021 pdf verification
- #Timely filing limit for all insurance 2021 pdf code
#Timely filing limit for all insurance 2021 pdf portable
The explanation is called the Remittance and Status (R&S) Report, which may be received as a downloadable portable document format (PDF) version or on paper. Claims filed under the same National Provider Identifier (NPI) and program and ready for disposition at the end of each week are paid to the provider with an explanation of each payment or denial.TMHP verifies all required information is present.Medicaid claims are subject to the following procedures: 2, Provider Handbooks) for more information about carve-out services. Refer to: The Medicaid Managed Care Handbook (Vol. Only claims for those services that are carved-out of managed care can be submitted to TMHP.Ĭlaims for EVV services (Acute Care and Long Term Care Fee-For-Service and Long Term Support Services ) must be submitted to TMHP to perform the EVV claims matching process and forwarded to the applicable payer for adjudication. Note:Claims for services rendered to a Medicaid managed care client must be submitted to the managed care organization (MCO) or dental plan that administers the client’s managed care benefits. TMHP processes claims for services rendered to Texas Medicaid fee-for-service clients and carve-out services rendered to Medicaid managed care clients.
#Timely filing limit for all insurance 2021 pdf code
The EVV aggregator will perform EVV claims matching and TMHP will forward the EVV claim with the EVV match code to the applicable payer for claims processing. Paper claims for EVV services will not be accepted.
#Timely filing limit for all insurance 2021 pdf verification
Providers are not allowed to bill clients or Texas Medicaid for completing these forms.Īll claims for Electronic Visit Verification (EVV) services, including fee-for-service and managed care claims, must be submitted electronically to TMHP using the appropriate electronic claims submission method. The client presents these forms to the provider. Medicaid providers are also required to complete and sign authorized medical transportation forms (e.g., Form H3017, Individual Transportation Participant Service Record, or Form 3111, Verification of Travel to Healthcare Services by Mass Transit) or provide an equivalent (e.g., provider statement on official letterhead) to attest that services were provided to a client on a specific date. Only claims for services rendered are considered for payment. Providers cannot bill Texas Medicaid or Medicaid clients for missed appointments or failure to keep an appointment. The cost of claims filing is part of the usual and customary rate for doing business.
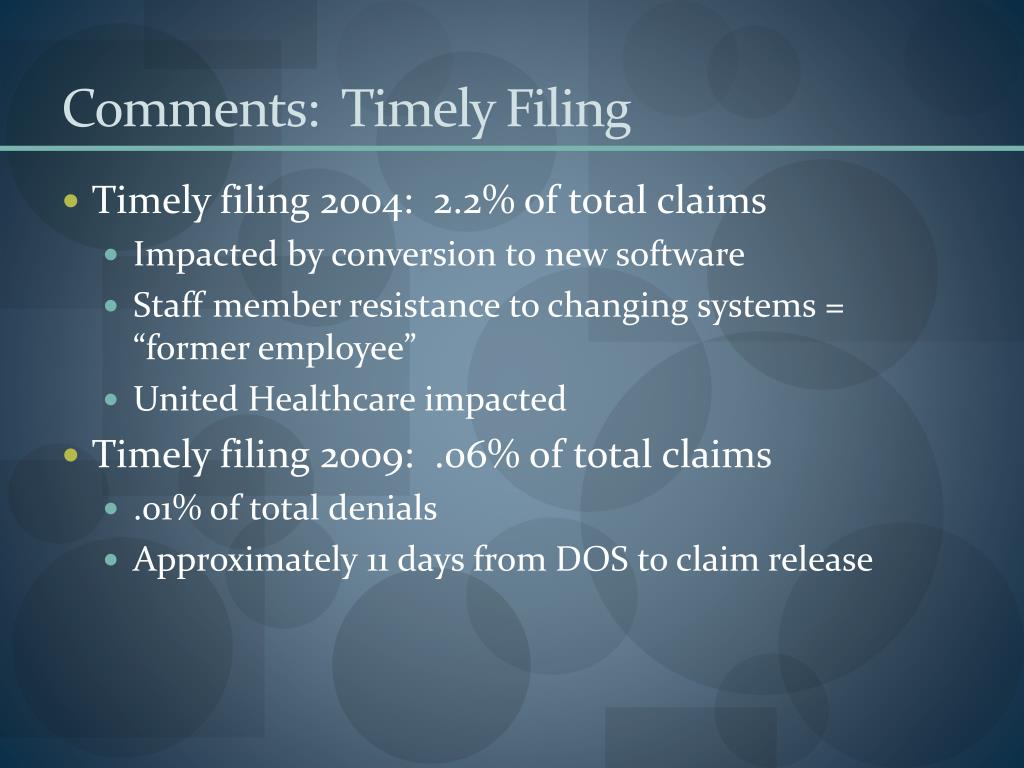
Providers are not allowed to charge TMHP for filing claims. Federal regulations prohibit providers from charging clients a fee for completing or filing Medicaid claim forms. Texas Medicaid does not make payments to clients. In case, you’re looking for some additional information, feel free to contact us or comment below.Providers that render services to Texas Medicaid fee-for-service and managed care clients must file the assigned claims. In this article, I have mentioned everything you need to know about timely filing limit along with the timely filing limit of all major insurances in United States. Also ask your accounts receivable team to follow up on claims within 15 days of claim submission. If insurance company allows electronic submission then submit claims electronically and keep an eye on rejections. To avoid timely filing limit denial, submit claims within the timely filing limit of insurance company.
#Timely filing limit for all insurance 2021 pdf how to
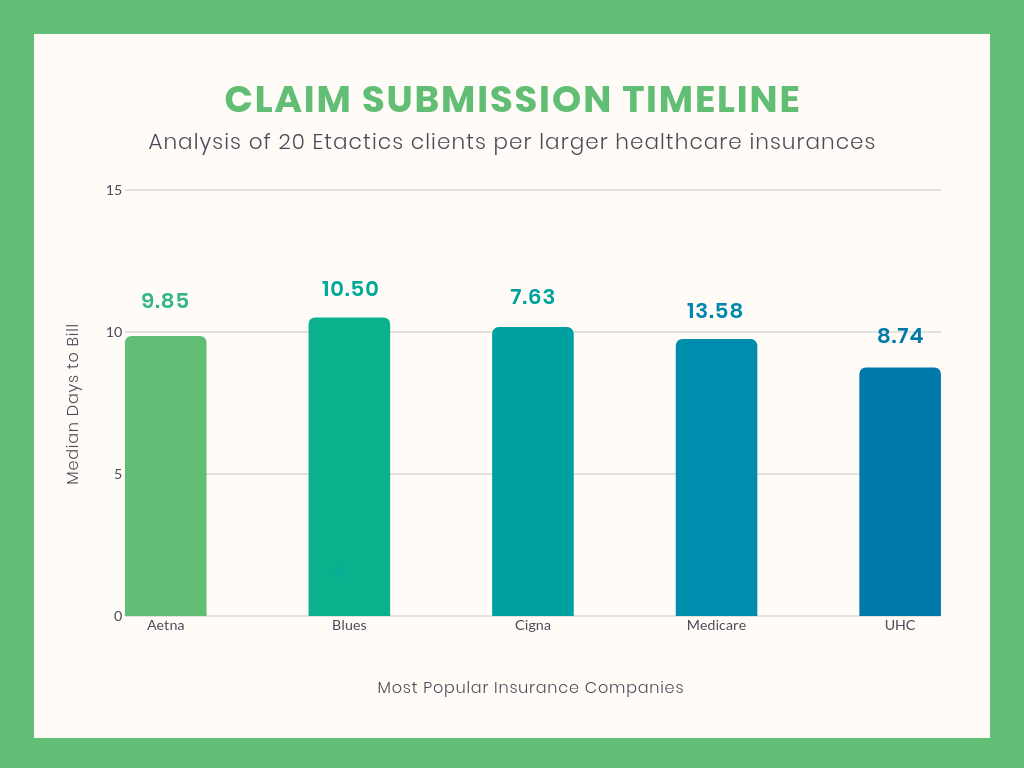
How to avoid from claim timely filing limit exhausted? What if claim isn’t sent within the timely filing limit?įailing to submit a claim within the timely filing limit may result in the claim being denied with a denial code CO 29, so it is important to be aware of the deadline and submit the claim promptly. Unitedhealthcare Non Participating Providers Keystone First Resubmissions & Corrected Claimsġ80 Calender days from Primary EOB processing dateġ2 months from original claim determination Amerigroup for Non Participating Providers


 0 kommentar(er)
0 kommentar(er)
